NIH grant to support continuing research on exercise and bone quality
More than 50 million Americans have osteoporosis, which is responsible for two million broken bones and $19 billion in related costs every year.
Exercise is one of the best defenses against low bone mass, but it’s not an equal-opportunity improver — different people and different bones respond differently to the mechanical stimulus provided by various forms of exercise.
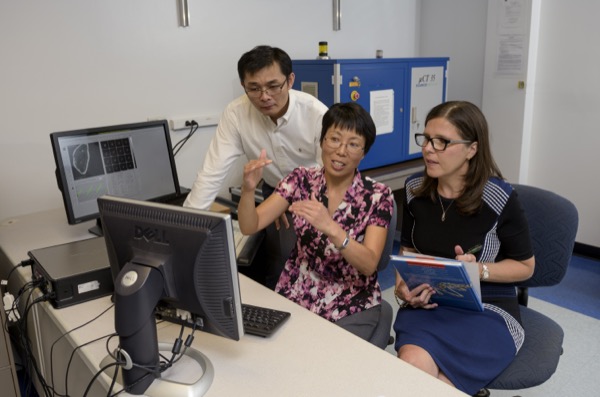
Now, new research by a multidisciplinary team led by the University of Delaware’s Liyun Wang may pave the way to identifying new molecular targets for preventing and slowing the onset of osteoporosis.
The work, which is funded through a five-year $1.9-million grant from the National Institutes of Health, may also help in the development of patient-specific exercise regimens to improve bone health.
Exercise can improve bone health by triggering the movement of fluid, nutrients and other factors in bone that keep bone cells happy and functioning.
Wang, associate professor of mechanical engineeringat UD, is partnering on the work with Cindy Farach-Carson (Rice University), Lucas Lu (UD, mechanical engineering), Catherine Kirn-Safran (UD, biological sciences) and Sherry Liu (University of Pennsylvania).
The award is a competitive renewal of Wang’s previous NIH grant on transport mechanisms in mineralized bone.
Her research group has successfully developed and validated a novel method to study the fluid flow-based delivery of various types of nutrients to osteocytes, the most abundant bone cells buried in bone.
Most importantly, the novel method allows them to probe the cellular apparatus that osteocytes use to detect outside exercise signals, at the submicron level for the first time. The method combines a sophisticated technique called FRAP (fluorescence recovery after photobleaching) with mathematical modeling.
Wang explains that osteocytes are critical to the maintenance of tissue quality and mechanical integrity of bone. As the primary exercise sensing cells, osteocytes orchestrate bone’s adaptation processes and tell the other bone cells whether they should make new bone or not.
To do this, osteocytes rely on information they receive from an array of suspension cables that anchor the cell body with the surrounding bone matrix wall. During exercise, fluid is squeezed between the cells and their surrounding walls, blowing the cables and transferring mechanical signals into the cells.
“Specifically, we want to know how perlecan, an extracellular protein that comprises part of the suspension cables, facilitates bone cell responses to mechanical loading,” Wang says.
In Wang’s previous research, she and her collaborators discovered that perlecan is needed to maintain the normal density of the suspension cables and to ensure positive responses to exercise. These preliminary studies formed the basis for their hypothesis that the osteocytic pericellular matrix of the cables regulates bone adaptation to exercise and other mechanical cues.
They now plan to test that hypothesis at the tissue, cellular and molecular levels.
“The pericellular matrix of the cables is critically positioned between the osteocytes and the hard part of bone,” Wang says. “Identifying the functions of the fluid sensing cables and one of its major components, perlecan, could lead to new strategies for regulating the sensitivity of osteocytes to mechanical loading during exercise.”
The work has the potential to improve the prevention and treatment of osteoporosis and advance fundamental knowledge about the pericellular matrix, a uniquely functioning but often overlooked structure found in nearly all mammalian cells.
“Prof. Wang has assembled an impressive interdisciplinary team for this research,” says Suresh Advani, George W. Laird Professor and mechanical engineering department chair. “With their complementary expertise, they are well positioned to pursue this challenging research, which has the potential to have a significant impact on health care.”